Herniated intervertebral discs are more often manifested in age-related osteochondrosis due to the dryness and fragility of the fibrous ring. But that's just one of the risk factors. Others include:
- Heavy load on the lumbar region due to overweight.
- Weakness of the muscular apparatus.
- Heredity.
- A sedentary lifestyle and, as a result, constant compression of the vertebral structures.
- Smoking.
- Excellent physical activity.
According to medical statistics, this disease occurs in men much more often than in women.
What are the most common causes of the disease:
- Injuries caused by traffic accidents or falls.
- Lift heavy objects with poor load distribution.
- Scoliosis or lordosis, causing increased stress on certain areas of the spine.
- Hip joint dysplasia.
- Chronic diseases, including tuberculosis of the spine, neoplasms, syphilis.
- Metabolic disorders (hereditary and acquired).
All of these factors cause the cartilage and bones of the spine to wear down and weaken. And this is the main reason for intervertebral hernia.
Stages of disease development
Without proper treatment, the disease progresses and the condition of damaged intervertebral discs worsens. There are four stages in the development of the disease:
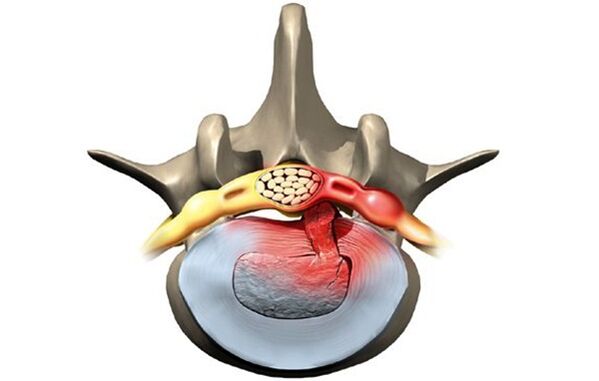
- Prolapse. The intervertebral disc has moved quite a bit, no more than two millimeters. The nucleus pulposus does not protrude from the vertebral body.
- Lumbar protrusion. The edge of the disc extends beyond the vertebral body to a distance of 1. 5 mm, but the displacement of the nucleus is not observed.
- Extrusion. The nucleus protrudes from the vertebral body.
- Sequestration. The nucleus practically falls and hangs above the vertebra in the form of a drop. At this stage, there is a risk of rupture of the fibrous ring and leakage of fluid secretion.
At the first stage of the disease, a person hardly worries about anything, sometimes there is back pain, but it quickly goes away. With the development of the disease, the state of health also worsens, the symptoms become more painful and alarming. If the diagnosis is not made in time and treatment is not started, the consequences are possible: paralysis of the legs and serious disorders of the nervous system.
How does a lumbosacral hernia manifest itself?
An intervertebral hernia can present with the following symptoms:
- Pain in the lumbar region.
- Pain when walking, radiating to the thigh area.
- Numbness of the feet, fingers, surface areas of the lower leg and thigh.
- Feeling of heaviness in the legs.
- Rigidity of movement.
In order not to delay in seeing a doctor, it is worth more carefully analyzing the symptoms of the disease. They can be divided into three groups.
Pain syndrome
Pain with a lumbosacral hernia is a key symptom. Even at the first stage, there is pain in the area of the damaged disc, especially after an injury. They may increase or decrease and then reappear. Most often, the sacred region does not even hurt, but hurts, especially during physical exertion or prolonged sedentary work. If a person lies on a healthy side and bends his leg, the pain goes away completely. This condition can last for several months.

With prompt treatment for medical help, it is easy to get rid of the problem. Just say goodbye to bad habits and do the physiotherapy exercises recommended by your doctor.
Every day, the affected area will increase, and the condition of the disc tissues will worsen. The transition to the second degree of the disease is signaled by increased pain. It is now felt not only in the sacral region, but covers the entire lower back, radiates to the cervical region, to each spinal muscle, buttocks, thighs, legs, feet and toes. Discomfort is manifested by even insignificant physical activity - coughing or sneezing.
Vertebral syndrome
The increase in pain in the second stage is accompanied by constant spasms of the back muscles. This leads to even greater discomfort for the patient. He cannot move freely, straighten his back, stretch. The gait of such a person becomes uncertain, he always leans towards the side opposite the patient, slumped.
Due to poor coordination of movements, the quality of human life deteriorates. He cannot perform defined tasks well at work, and active rest due to constant pain becomes unrealistic.
Radicular syndrome
If a hernia is left unattended by doctors, progressive disease causes compression of the spinal roots, leading to their death, and blood access to the tissues of the damaged disc is almost impossible. Symptoms characteristic of severe stages of the disease appear:
- Weakening of the leg muscles. The patient cannot squat, stretch, jump. Even climbing the stairs is difficult for him.
- Numbness of the affected area and surrounding areas. The skin becomes numb and pale, there is a sensation of goosebumps and tingling. Patients complain of hyperhidrosis in the affected area and legs, or, on the contrary, excessive dryness of the skin.
- Lumbago. The patient suffers from lumbago in the lumbar region with sharp, sharp pain, which increases with any movement. If left untreated, it leads to destruction of the hip and knee joints.
- Noticeable thinning of the painful leg, resulting in asymmetry of posture.
- Disruption of the pelvic organs. The urological and gynecological affections are aggravated, the libido disappears, diarrhea, urinary incontinence are possible.
In severe cases of spinal hernia, there is a risk of paralysis, disability, and even death.
Pathology diagnosis
If a person suffers from severe lower back pain, they should make an appointment with a neurologist. He will carry out an examination with medical examinations:
- Identification of the reflexes of the tendons of the lower limbs.
- Leg lift test.
- Determination of sensitivity to heat or cold, pain and vibration over the entire surface of the legs, thighs, buttocks, stomach and back.
The doctor will then refer the patient for an MRI or CT scan of the lumbar spine. Using tomographic techniques, a three-dimensional image of the affected area will be obtained. It can be used to determine the location and size of the hernia, the stage of the disease.
If there is a risk of spinal cord injury, electromyography, neurography, and contrast myelography are also prescribed. Using these studies, the doctor will determine if urgent surgery is needed.
Herniated disc treatment
A spinal hernia is treated both conservatively and surgically. The choice of technique depends on the stage of development of the disease, the presence of concomitant diseases and contraindications.
Conservative therapy
The therapeutic course is aimed primarily at relieving pain and alleviating the patient's condition.
What pharmaceuticals can a doctor prescribe:
- Medicines that relieve pain and inflammation. In case of exacerbation - in the form of injections. When the acute pain is relieved (usually three to four days is enough), oral medications with a similar effect are prescribed.
- Blockage of novocaine with the addition of corticosteroids. A similar method is able to stop the pain for two weeks at a time. Usually a series of blockages are performed with injections into different parts of the damaged disc.
- Centrally acting muscle relaxants. They reduce muscle activity by relieving painful cramps.
- Vitamin and mineral complexes with emphasis on elements of group B. They slightly relax muscles, help tissue regeneration and conduction of nerve impulses.
After the pain syndrome is relieved, the consumption of pharmaceuticals decreases. Treatment of the disease is based on physiotherapy and physiotherapy.
Physiotherapy treatment methods are also chosen depending on the patient's condition. It could be :
- Treatment with heat or electric shock.
- Electrophoresis with anti-inflammatory drugs.
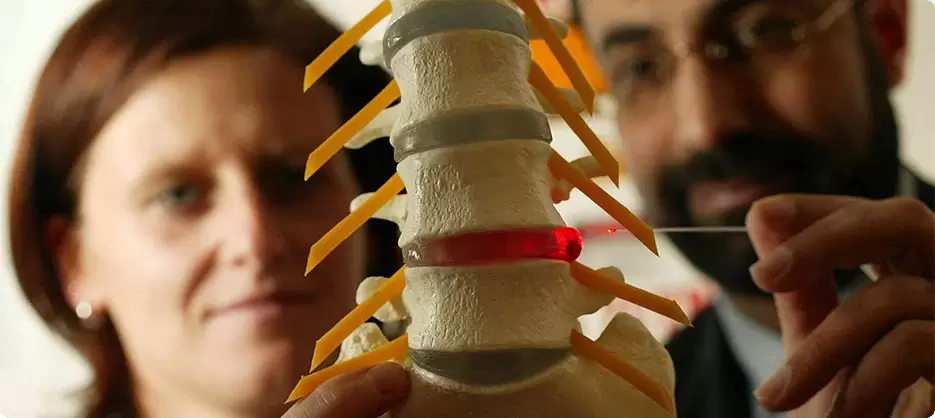
- Acupuncture and acupressure.
- Hirudotherapy.
- Hydromassage.
Normal massage is allowed only if there is no pain syndrome. A more effective physiotherapy treatment is manual therapy with post-isometric relaxation.
Doctors strongly recommend that smoking patients quit smoking.
Nutritional adjustments are also important, especially for overweight patients. Fatty, salty, sweet and alcoholic dishes must be excluded from the menu. Eating a sober diet with an abundance of vegetables and fermented dairy products will help the body to cope better with the treatment, as well as get rid of the pounds that are weighing on the back.
Surgical intervention
Conservative treatment usually lasts about two months. If this does not give the desired result, a decision is made to change the therapeutic tactics or to perform surgery. The latter is prescribed for severe pain, loss of sensitivity in the legs, dysfunction of the pelvic organs. Depending on the complexity of the situation, the operation is carried out as follows:
- Endoscopic method. Three micro-incisions are made in the affected area. A camera is inserted into one to broadcast to the monitor. Through the other two, the protrusion of the hernia is removed with the help of miniature instruments.
- By the percutaneous discectomy method. The damaged nucleus is removed by a puncture in the spinal disc and replaced with an artificial substance.
- By laser reconstruction. It is performed in the form of punctures using a special needle without dissecting the tissue. The laser radiation heats the structures of the disc and stimulates cell regeneration, while relieving pain.
In difficult cases, endoprosthesis of the vertebral discs is possible - replacing the damaged organ with an implant.

After complex surgeries, rehabilitation will be necessary. The operated person will need to wear a corset and will not be able to sit up for about three months. An additional period of rehabilitation involves the practice of therapeutic gymnastics and physiotherapy.
Preventive techniques
Like any other disease, herniated discs are easier to prevent than to cure. What you need to do to keep your spinal discs healthy:
- Calculate loads accurately if your job is related to it or if you are a professional athlete.
- Correct body weight (its index should not exceed 30).
- Choose a good mattress to sleep in the right position (preferably on your back).
- Practice gentle physical education, swimming, fitness.
- Include exercises in morning exercises to strengthen the muscle corset of the spine.
- Give up smoking.
- Eat well.
If observing these rules becomes a habit, there is a risk of contracting a spinal hernia only as a result of an accident.
A herniated disc is dangerous with serious consequences, and the treatment of advanced cases is very long. To avoid surgery and complications, if you have painful sensations in your back, you should see a neurologist.
Osteochondrosis
The term osteochondrosis itself is derived from two words: osteo - bone and chondrue - cartilage. Simply put, it is the ossification of the cartilage. Although this interpretation is fundamentally wrong. Some in their delusions go even further and are convinced that osteochondrosis is the deposit of salts in the joints. In addition, it is table salt that is supposed to be consumed in large quantities.
Pathogenesis
In reality, everything turns out a little differently. And harder. And table salt, if it plays any role in the development of osteochondrosis, is very indirect. Osteochondrosis is based on dystrophy and degeneration of the articular cartilage. This is not an independent disease, but a pathological process that can be noted almost anywhere there is connective cartilage tissue.
Still, osteochondrosis in the overwhelming case affects the spine. Why is that? The fact is that between the vertebrae there is a kind of spacers - the intervertebral (intervertebral) discs. The physiological role of these discs is to cushion and protect the vertebral bodies from premature wear due to mechanical stresses. The disc consists of an internal liquid nucleus pulposus surrounded by a fibrous ring and an upper and lower plate.
The disc undergoes enormous mechanical stress, resulting in permanent damage to its structures at the cellular level. In humans, these processes are too pronounced - this is our compensation for standing walking. To prevent the disk from being completely "erased", it must be constantly regenerated, that is, restored. It is the balance of damage regeneration processes that determines the normal structure of the intervertebral disc. Another curious detail is that the supply of blood and nutrients to the intervertebral discs takes place not through the blood vessels, which are invaded by growth in childhood, but in a diffuse way, from the bone tissue of the vertebral bodies. . Again, the payment for the ability to walk on two limbs, not four.
As a result, the intervertebral discs are easily injured in anatomical and physiological terms. Any negative process in the body leads to an imbalance in the regeneration of damage and the development of dystrophy and degeneration of the discs. A structurally defective disc is no longer able to withstand the appropriate mechanical stresses. Under excessive pressure from the overlying vertebrae, the discs are moved in different directions, usually to the sides and back. This process is called a herniated disc.
The bone tissue of the vertebrae, which has lost its cartilage lining, also undergoes mechanical wear. Due to constant trauma on the surface of the anterior edge of the vertebral bodies, pathological bone growths are formed - osteophytes. Spondylosis develops. Due to the degeneration and displacement of the disc, the intervertebral spaces decrease, the spinal canal narrows, and the roots of the spinal nerves are violated in what is called. foraminal holes.
Causes
The causes, or etiological factors, of osteochondrosis are diverse. They can be both local, that is, caused by the pathology of the spine itself and general disorders at the level of the organism. Any pathology leading to a violation of the structure of the spine or metabolic disorders can be considered the cause of osteochondrosis. In this regard, there are:
- Changes in the configuration of the spine (scoliosis, pathological lordosis or kyphosis)
- Other defects of the musculoskeletal system - flat feet, narrow shoulder girdle, pelvic abnormalities
- Spinal injury
- Low immunity
- Metabolic disorders - osteoporosis, obesity, diabetes mellitus, thyroid disease
- Diseases of the cardiovascular system - atherosclerosis, hypertension
- Digestive disorders leading to insufficient absorption of nutrients from the gastrointestinal tract
- Heredity.
It should be noted that the above pathological conditions do not necessarily lead to osteochondrosis. It requires constant exposure to certain predisposing factors - hypothermia, malnutrition, sedentary lifestyle or, on the contrary, excessive physical exertion.
Symptoms
Osteochondrosis itself is an asymptomatic process. And at the same time, the signs of degeneration of the intervertebral discs are various. How? 'Or' What? The fact is that the clinical manifestations of osteochondrosis are based on its complications - herniated discs, spondylosis, sciatica, narrowing of the spinal canal.
In addition, the clinic is very variable depending on the predominant location of the process in the cervical, thoracic or lumbosacral spine. The last section is most often affected, since it is the lower back that exercises the most physical activity. Signs of osteochondrosis of the lumbosacral region:
- Pain (lumbodynia, lumbago, sciatica)
- Restriction of movement in the lower back and lower limbs (intermittent claudication)
- Here, paresthesia-type sensitivity disorders - numbness, burning, crawling
- Pathological tension of the lumbar muscles
- In the absence of treatment, disorders of the function of the pelvic organs.
Cervical osteochondrosis is observed somewhat less frequently than lumbosacral. However, this pathology is also quite common. In addition to the typical signs of pain (neck pain), decreased sensitivity and movement of the upper extremities, cervical osteochondrosis due to insufficient blood supply to the brain has its own characteristics. These characteristics are manifested:
- Insomnia
- Headache, dizziness
- Periodic nausea
- General weakness, rapid fatigue
- Blood pressure fluctuations
- Sometimes toothache
- Behavioral reactions in the form of crying, irritability.
The thoracic region with osteochondrosis is relatively rarely affected. Patients in this case are people who are forced to sit in a fixed uncomfortable position by profession - students, schoolchildren, programmers, office workers. Symptoms of osteochondrosis in this case will be as follows:
- Pain and paresthesia in the chest
- Dyspnea
- Heartbeat feeling
- Restriction of movement in the thoracic spine.
Diagnostic
From all this it is clear that osteochondrosis is a chameleon disease. Due to the similarity in signs, it is easy to confuse it with stroke, hypertension, myocardial infarction, angina, neurotic disorders. That is why, in order to make the correct diagnosis, a complex and comprehensive diagnosis is necessary in order to correctly determine the symptoms and treatment of osteochondrosis.
This diagnosis, in addition to the traditional questioning and clarification of patient complaints, should include special medical examination and research methods. These methods include x-ray of the spine, ultrasound of internal organs. Recently, magnetic and computed resonance imaging have been used successfully to diagnose osteochondrosis.
Processing
Therapeutic tactics for osteochondrosis involve the use of:
- Medications
- Massage
- Physiotherapy procedures
- Physiotherapy (exercise therapy)
- Manual therapy
- Acupuncture.
Medicines for osteochondrosis are primarily aimed at relieving pain and eliminating inflammatory processes in the nerve roots. For this purpose, NSAIDs drugs are used. In various combinations, these drugs are widely used in the form of ointments, injections, tablets for the treatment of osteochondrosis. It should be remembered that these drugs have a negative effect on the liver, stomach and intestines. In doing so, they can worsen the metabolic disorders in osteochondrosis. They relieve the pain of the blockade well with local anesthetics. True, the effect of these funds is short-lived and in no way affects the course of osteochondrosis as a whole.
It is possible to improve metabolic processes locally and in the body with the help of drugs such as chondroprotectors, immunostimulants and vitamins with minerals. Chondroprotectors are used in tablets, ointments and ampoules. Among the fortifying agents, vitamins C, group B, in combination with minerals are used. In this regard, calcium preparations are most preferred. Indeed, contrary to some erroneous claims, the basis of osteochondrosis is not an excess, but just a deficiency in Calcium.
After successfully relieving the exacerbation, physiotherapy, massage and exercise therapy are presented. Calcium electrophoresis, hydrocortisone phonophoresis, amplipulse, paraffin therapy are used as physical procedures. All of these measures are aimed at eliminating pain and inflammation of the nerve roots, ligaments and muscles. Massage for osteochondrosis is carried out according to the generally accepted method. The massage area is chosen depending on the location of the osteochondrosis. Expansion of range of motion is achieved with the help of exercise therapy. At first, in the phase of exacerbation, there are practically no dynamic loads. The patient is constantly in an optimal posture. At this stage, it is desirable to wear immobilization devices - a lumbar corset, a Shant's collar. As the exacerbation is suppressed, the volume and duration of movements during exercise therapy increase.
Recently, in the treatment of osteochondrosis, non-traditional methods of treatment have been received - acupuncture, manual therapy, osteopathy. Acupuncture is an effect on special biologically active points located along the spine, on the atria, on the hands and on the feet. With manual therapy, the normal position of the vertebrae and intervertebral discs is restored through the manual action of the hands of a specialist. And during osteopathy, the structural integrity of the musculoskeletal system is ensured by specific techniques. In the absence of the effect of conservative measures for the treatment of osteochondrosis, persistent pain, complications, surgery is indicated. The pathologically displaced disc is removed. Currently, for this purpose, a microdiscectomy is performed - the endoscopic removal of a displaced disc.



































